Frequent Urgency to Urinate: a Warning Signal
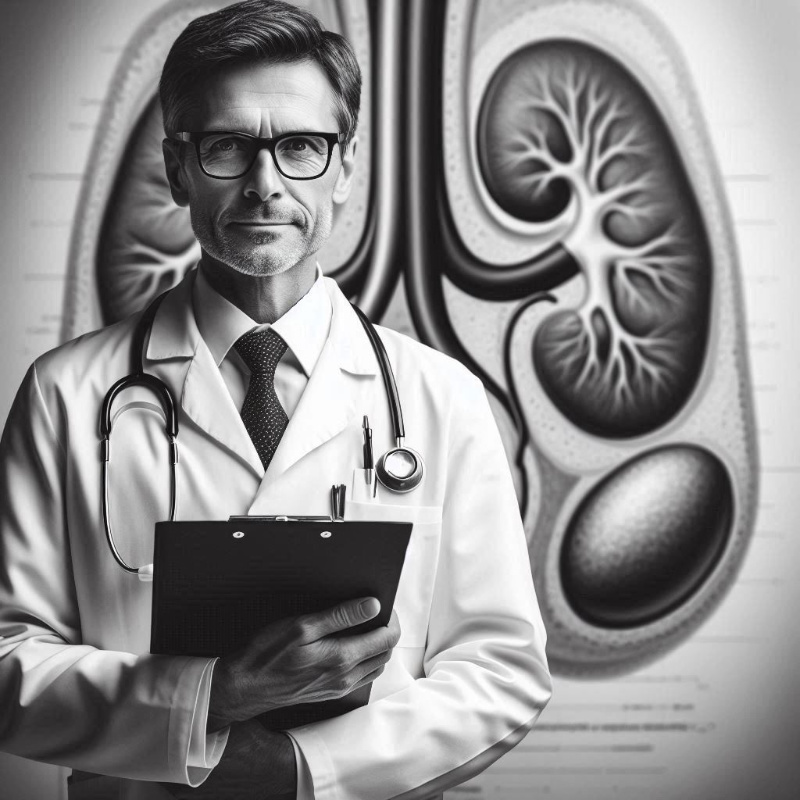
A sudden increase in the urgency to urinate can often be dismissed as a minor inconvenience, but it may signal the onset of Prostatic Hyperplasia, a condition characterized by the enlargement of the prostate gland. This gland surrounds the urethra, the duct through which urine exits the body. As the prostate enlarges, it can exert pressure on the urethra, resulting in the urge to urinate more frequently. This symptom is far from an isolated nuisance; it is a red flag indicating that the body is experiencing underlying changes warranting medical attention.
The biological underpinnings of this urgency stem from the pressure applied by the enlarged prostate on the bladder and urethra. This pressure compromises the bladder's ability to hold urine efficiently and creates an almost constant urge to urinate, even when the bladder is not full. The science behind these mechanics is clear: the disruption in the normal flow and storage of urine signals potential prostatic hyperplasia.
Moreover, the frequent need to urinate, particularly if disrupting daily life or sleep patterns, should prompt an assessment for Prostatic Hyperplasia. It's crucial to understand that this condition progresses over time. Early detection and management are vital in mitigating the impact on quality of life and preventing complications. Engaging with a healthcare provider for screening and potential diagnostic tests is a proactive step toward maintaining urinary health.
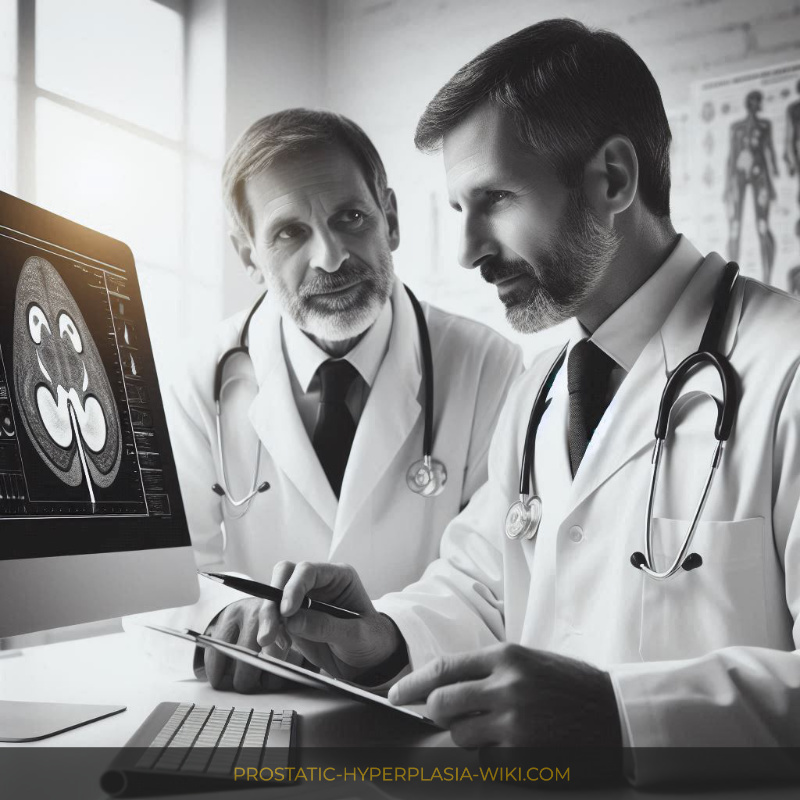
Investigations into this symptom often include a thorough medical history assessment, physical examinations, and may involve tests such as urine analysis or ultrasounds to evaluate the prostate's size and shape. Here is a brief overview of some diagnostic tools:
| Diagnostic Tool | Use |
|---|---|
| Medical History & Physical Exam | Assesses symptoms and physical signs of Prostatic Hyperplasia. |
| Urine Analysis | Evaluates urinary tract infections or other urine abnormalities. |
| Ultrasound | Provides imaging of the prostate, identifying enlargement or obstructions. |
Conclusively, while the initial reaction may be to dismiss increased urination urgency, it is a pertinent symptom of a more significant health issue. Early intervention and treatment can alleviate symptoms, improve life quality, and potentially stave off more severe complications.
Difficulty Starting Urination: Not Just Aging
Many individuals may mistakenly attribute the difficulty in initiating urination to the natural aging process, dismissing early signs that could indicate a more significant underlying condition. However, this symptom often heralds the onset of prostatic hyperplasia, a benign enlargement of the prostate gland that disrupts the normal flow of urine. As the prostate enlarges, it exerts pressure on the urethra, the tube carrying urine from the bladder outside the body, leading to challenges in starting the urination process. This phenomenon underscores the importance of discerning between standard age-related changes in bodily functions and symptoms that may signify prostatic hyperplasia.
Understanding the physiology behind this condition provides valuable insight into why it manifests in such a manner. The prostate gland, which plays a crucial role in male reproductive activity, surrounds the urethra. When the gland enlarges, a condition referred to scientifically as benign prostatic hyperplasia (BPH), it can constrict or partially block the urethra. This blockage is what leads to the symptom of hesitancy or difficulty commencing urination. It is a clear signal from the body that something is amiss, prompting a deeper investigation into potential prostatic issues.
Addressing this challenge requires a comprehensive diagnostic approach to confirm whether what is being experienced is indeed due to prostatic hyperplasia. Medical professionals may employ a variety of diagnostic tools, including digital rectal exams, urine tests, and ultrasounds, to evaluate the extent of prostate enlargement and its impact on urination. Understanding that these symptoms are not merely an inevitable consequence of aging but could indicate a treatable medical condition is pivotal in seeking timely and appropriate intervention, improving the quality of life.
A Weak or Interrupted Urinary Stream Unveiled
A weakened or interrupted urinary stream is often a tell-tale sign that should not be dismissed lightly. At the heart of this condition lies Benign Prostatic Hyperplasia (BPH), a common affliction that enlarges the prostate gland and encroaches upon the urethra, impeding the flow of urine. The mechanics of micturition, or urination, become compromised, eliciting a stream that is not only weak but may also start and stop abruptly. This symptomatology is reflective of the underlying obstruction within the urinary tract, highlighting the urgency for a clinical assessment.
Diving deeper into the dominion of what is prostatic hyperplasia reveals an intricate interplay of hormonal changes, specifically a notable increase in dihydrotestosterone (DHT) levels within the prostate. This hormonal surge stimulates prostate growth, which then presses against the urethra, acting as a partial blockade. The detrusor muscle of the bladder must exert more force to expel urine through the narrowed passage, often leading to the weakening of these muscles over time. Consequently, the bladder cannot fully empty, setting the stage for further complications including urinary retention and the increased risk of urinary tract infections.
The significance of recognizing a weakened or interrupted stream extends beyond discomfort; it serves as a harbinger for potential health deterioration if left unchecked. Early detection and intervention can significantly mitigate the progression of BPH, incorporating lifestyle alterations, pharmacotherapy, and, in certain scenarios, surgical procedures to relieve symptoms. Moreover, understanding the etiology of BPH underscores the importance of routine medical check-ups for men, especially as they age, to ensure optimal urinary tract health and the preemptive addressing of any signs indicative of prostatic hyperplasia.
The Unseen Culprit: Urinary Retention Explained
Urinary retention, characterized by the inability to completely empty the bladder, emerges as a pivotal concern in patients grappling with prostatic hyperplasia. This condition, where the prostate gland enlarges, impeding the flow of urine, remains a silent harbinger of potential complications if left unaddressed. The intricacies of this phenomenon delve deep into the realms of urological health, spotlighting the significance of understanding its underpinnings. At the core, the mechanism involves an encroachment upon the urethra by the enlarged prostate, 
As knowledge about what is prostatic hyperplasia broadens, the imperative for early detection and management of urinary retention assumes paramount importance. Symptoms can subtly manifest, initially overshadowed by the body's attempts to compensate for the impeded urinary flow. However, as the condition progresses, the bladder may begin to demonstrate a diminished capacity to contract and expel urine, leading to residual urine volume that exacerbates the risk of infections and bladder stones. The clinical landscape thus necessitates a proactive approach, intertwining diagnostic acumen with therapeutic strategies aimed at alleviating obstruction and restoring urinary function.
The confluence of advanced diagnostic modalities and treatment options illuminate a path forward in addressing urinary retention associated with prostatic hyperplasia. From pharmacological interventions aiming to reduce prostate size to surgical techniques designed to remove the obstruction, the arsenal against this condition is robust. Furthermore, patient education on recognizing early signs of urinary retention fosters a collaborative effort in managing prostatic hyperplasia effectively. It underscores the essence of timely medical consultation to circumvent potential complications, reinforcing the importance of an informed patient population in combating the nuances of urological disorders.
Nocturia: Disturbed Sleep Due to Frequent Nighttime Urination
In the quiet hours of the night, many individuals find themselves repeatedly journeying from bed to bathroom, a situation that is far from normal and often indicative of underlying health conditions such as prostatic hyperplasia. This condition, characterized by the enlargement of the prostate gland, significantly impacts the lower urinary tract, leading to nocturia. Not merely an inconvenience, nocturia disrupts sleep patterns and can have a profound impact on an individual's quality of life. The interruption of the sleep cycle inhibits the body from entering deeper, restorative stages of sleep, leading to daytime fatigue, decreased productivity, and even an increased risk of accidents or falls, particularly in older adults.
Understanding nocturia requires a dive into the mechanisms at play. The process of normal urination involves a complex interplay between the kidneys, bladder, and various neural pathways, all of which can be compromised by prostatic hyperplasia. As the prostate enlarges, it can impinge upon the urethra, leading to bladder outlet obstruction. This obstruction not only makes it difficult for the bladder to empty completely during urination but can also stimulate an overactive bladder at night, when the body is positioned horizontally. Consequently, the bladder sends frequent signals of fullness to the brain, even when it may not be entirely full.
| Condition | Description | Relevance to Nocturia |
|---|---|---|
| Prostatic Hyperplasia | Enlargement of the prostate gland causing urinary symptoms | Directly contributes to nocturia by causing bladder outlet obstruction and affecting the normal urinary flow. |
| Bladder Overactivity | The bladder muscle's inability to properly control urination | Can lead to nocturia by causing frequent urges to urinate, especially at night. |
| Urinary Tract Infections | Infections that can affect any part of the urinary system | While more indirectly, can exacerbate nocturia by increasing urinary frequency and urgency. |
For those grappling with nocturia, it is crucial not to dismiss these nightly interruptions as mere inconveniences or inevitable consequences of aging. They may be early harbingers of prostatic hyperplasia, signaling the need for a thorough medical evaluation. Recognizing and addressing nocturia can not only improve sleep quality but also mitigate the adverse effects this condition can have on overall well-being and health.
Urinary Tract Infections: a Recurring Battle
In the complex dialogue between urinary health and prostatic hyperplasia, urinary tract infections (UTIs) emerge as frequent yet often underestimated adversaries. These infections are not just simple, isolated occurrences but are intricately linked with the underlying condition of an enlarged prostate. The prostate, when enlarged, can impede the flow of urine, creating an environment conducive to bacterial growth and making UTIs a recurrent battle for many. This is not merely a matter of discomfort but of significant concern, as repeated UTIs can lead to more severe complications, including kidney damage.
The pathophysiology behind this recurrent cycle of infection is rooted in the incomplete emptying of the bladder. As urine stagnates, it becomes a breeding ground for bacteria, escalating the risk of infection. The situation is exacerbated by the fact that an enlarged prostate can essentially act as a barrier to urine flow, complicating the body's natural ability to flush out pathogens. Despite the body's attempts to counter these infections through immune responses, the compromised urinary flow often undermines these efforts, leading to the cyclical nature of UTIs in the context of prostatic hyperplasia.
Addressing this issue requires a nuanced approach that goes beyond the symptomatic treatment of UTIs. The management strategies must encompass not only the eradication of the infection through antibiotics but also interventions aimed at restoring normal urinary flow and reducing prostate size, if medically advised. Lifestyle modifications, including increased fluid intake, cranberry supplementation, and bladder training, can also play supportive roles in mitigating the recurrence of UTIs by promoting a more complete bladder emptying and enhancing the urinary tract's defenses.
The recurrent UTIs associated with prostatic hyperplasia underscore the interconnectedness of urinary system health and call for an integrated approach to management. It is paramount for individuals experiencing these symptoms to engage with healthcare providers to develop a comprehensive plan that addresses both the acute infections and the underlying prostatic issues. Through a combination of medical treatment, lifestyle adjustments, and proactive healthcare engagement, it is possible to mitigate the impact of UTIs and improve overall urinary health in the context of prostatic hyperplasia.
Content Manager: Dr. Eric Klein